INTRODUCTION
The International Association for the Study of Pain (IASP) currently defines pain as “an unpleasant, sensory, emotional experience associated with, or resembling that associated with, actual or potential tissue damage”[1]. Pain is reputed to be the most common symptom to compel a patient to seek medical attention. Postoperative pain is acute pain produced by deliberate surgical trauma with an inflammatory reaction and initiation of an afferent neuronal barrage. It is a combined constellation of several unpleasant sensory, emotional, and mental experiences precipitated by surgical trauma and associated with autonomic, endocrine-metabolic, physiological, and behavioral responses. Adequate postoperative pain relief is a fundamental human right and optimal dynamic postoperative pain relief aids the resumption of normal physical and mental activities. It has been established that optimization of postoperative pain treatment will improve postoperative recovery, and decrease morbidity and length of hospitalization [2]. Cesarean section is one of the most common operative delivery procedures with an attendant substantial postoperative pain [3]. Studies have reported in the past 3 to 4 decades that 20 to 80% of patients undergoing surgery suffer from inadequately treated pain [4] and pain is classified as a serious public health problem both in the developed [5] and in developing countries [6]
Post-operative pain management following abdominal surgeries poses a challenge to anesthetists. Conventional practice involved the use of opioids as well as neuraxial analgesic techniques. Unfortunately, opioid-based analgesic methods are not without potential risks and side effects. These side effects include nausea, vomiting, pruritus, urinary retention, constipation, respiratory depression, and sedation. As a result, the management of perioperative pain has now taken the recommended model of multimodal or “balanced” analgesia technique using a combination of opioid, non-opioid analgesics, and local anesthesia to improve pain control and minimize opioid-related side effects [7]. The combination of multimodal techniques can reduce the side effects of opioids; and improve pain control, patient satisfaction, early ambulation, infant care, time to discharge, and early return to daily activities [8]. The availability and access to opioids in Nigeria have been erratic and coupled with its associated side effects; there has been a need for alternative techniques of analgesia. The Transversus abdominis plane (TAP) block could be a viable technique in the multimodal strategy.
The Transversus abdominis plane (TAP) block is relatively new, safe and with minimal side effect when compared to the routine high dose of opioid used in pain management. Doctors are encouraged to use this technique, especially as part of a multimodal approach to provide postoperative analgesia via the anterolateral abdominal wall [9]. TAP block involves a single large bolus injection of local anesthesia into the abdominal wall (TAP), an anatomical space between the internal oblique and transversus abdominis muscles. It blocks the branches of the lower 6 thoracic and upper lumbar nerves [10]. The primary outcome of this study is to compare the postoperative analgesic effects of TAP block and intravenous morphine using a visual analog scale (VAS). The secondary outcomes are to compare time to the first analgesic request between the two groups, side effects in the two groups following administration of TAP and systemic morphine, and the level of patient satisfaction with pain management between the two groups.
2. METHODOLOGY
2.1 Study Area and Period:
The study was conducted at LAUTECH Teaching Hospital, now UNIOSUN Teaching Hospital, Osogbo, Osun State, between September 1 and November 30, 2017. Osogbo has two local governments: Olorunda and Osogbo Local Government Areas. The town lies at latitude 70 and 460 north and Longitude 40 and 340 east. Its total land area is 47km2. Osogbo is accessible from any part of the state, and patients are referred to these hospitals. The city has a population of 156,694 people. LAUTECH Teaching Hospital is a tertiary health facility offering specialized and general healthcare to the people of Osun State and neighboring states.
2.2 Study design and population:
The study was a randomized controlled trial. Study information was provided to potentially eligible women of the American Society of Anesthesiologists (ASA) class I and II patients between the ages of 18-40 years scheduled for elective cesarean section via Pfannenstiel incision under spinal anesthesia.
2.2.1 Exclusion Criteria
Those excluded were patients with BMI >30kg/m2, cardiopulmonary disease, history of allergic reaction to local anesthetics, patients who refused to participate those with any contraindication to spinal anesthesia, patients with a previous scar, and patients with vertical incision.
2.2.2 Operative Techniques
Preoperative assessment was conducted at least 24 hours before surgery. Only patients with parameters within normal limits were included in the study. Blood was grouped and cross-matched. We instructed the patients to use VAS for pain assessment and they were told to request for analgesic when in pain. Patients were fasted overnight, premedicated with IV ranitidine 50mg and IV metoclopramide 10mg 1 hour before surgery. Patients were randomly allocated to undergo bilateral TAP block (n=40) with 20mls 0.25% plain bupivacaine on each side in group A or TAP block with 20mls normal saline (control n=40) on each side in group B. The allocation sequence was generated by a table of random numbers and group allocation was concealed in sealed opaque envelopes and put in a box. The envelope was picked up by the patient. A registrar in the department of anaesthesia coded the envelope against the labeled drugs according to the number. The researcher and the patient were blinded to the number in the envelope and the labeling of the test drug.
On the morning of surgery, an anesthetic checklist was done with preparation for resuscitation drugs, appropriate sizes of laryngoscopes, and different sizes of endotracheal tubes. The patient was moved to the theatre and positioned on the table with a right hip wedge (Crawford wedge) to ensure left lateral uterine displacement. The baseline vital signs were taken and recorded, and intravenous access was established with a wide- bore (16G) cannula. Patients were preloaded with 20ml/kg of normal saline over 10–15 minutes before the institution of subarachnoid block.
A multiparameter monitor was attached to monitor pulse rate, electrocardiography, peripheral oxygen saturation, and non-invasive blood pressure.
Each patient was placed in a sitting position with feet resting on a stool. Under strict asepsis, L3/4 or L4/5interspace was located using both iliac crests as landmarks at L4 interspace, a 26G Quincke spinal needle penetrated the space until a give was felt, after withdrawal of stylet and there was free flow of cerebrospinal fluid. Two milliliters of 0.5%hyperbaric bupivacaine (10mg) were injected into the subarachnoid space to provide a subarachnoid block.
The needle was removed, the puncture site was dressed in sterile gauze, and the patient was positioned supine with a 15-degree head-up tilt. All vital signs were recorded at 2-minute intervals for the first 20 minutes and then at 5-minute intervals until the end of surgery.
During the pre-incision period, the sensory block was assessed with cotton wool at a 2.5-minute interval until the block was assumed to be fixed, evidenced by none rising of the level of the block i.e. the sensory level. A sensory level between T4 and T6 was achieved in all the patients. Motor block was assessed using the Bromage Scale. A bromage score of 3 was acceptable for the surgical procedure to commence. On delivery of the baby, IV oxytocin bolus 2.5 IU was administered, and 5-10 IU of oxytocin in 0.5L of normal saline. The baby was subsequently given post-delivery care as dictated by the APGAR score at 1 and 5 minutes.
Blood loss was assessed by a visual estimate of swabs, and linen and by measuring the content of suction bottles.
Hypotension was defined as a mean arterial pressure (MAP) of less than 50mmHg or systolic pressure of less than 90mmHg [11]. Hypotension was treated with crystalloid infusion and when necessary, boluses of ephedrine 3-6mg were administered intravenously until hypotension was resolved. Bradycardia was defined as a pulse rate of less than 60 beats per minute [12] and was treated with IV atropine 0.6mg. Nausea and Vomiting were managed with intravenous ondansetron 4mg immediately after the cesarean section, a TAP block was instituted.
Procedure for TAP block
TAP block was performed by locating the triangle of petit. The triangle is above the iliac crest, which is the base, with the muscle of the external oblique forming the anterior border and latissimus dorsi the posterior border of the triangle. After identification of the triangle of petit, a blunt-tip 24gauge, 5.08cm (2-inches) needle was inserted perpendicular to the skin, midway between the iliac crest and the 10th costal margin at the mid- axillary line. The needle was advanced; two pops were felt, indicating the passage of the needle through the fascia extensions of the external oblique and internal oblique muscles. After the second pop the needle tip was assumed to be within the TAP and 20ml of 0.25% plain bupivacaine was deposited per side in Group A and 20ml of normal saline in Group B. The Patient was transferred to the postanaesthetic care unit (PACU) where pain scores were assessed along with standard monitoring until the patient was fit to be discharged from the PACU to the ward. Discharge criteria at PACU were determined using appropriate scores in the New Aldrete Scoring System and Visual Analogue Scale (VAS) as shown in Appendix 1. Patients transferred to the ward had at least 12 scores (no score less than 1 in any individual item) and VAS< 4.
The time of the first analgesia request (this was the time from the institution of the TAP block to the first analgesia request by the patient) was noted. The registrar that coded the envelope against the labeled drugs initially instructed the nurses on the ward to give I.M Diclofenac 75mg 12 hourly to patients in Group A as rescue analgesia. The patients in Group B had I.V morphine 4mg 4 hourly and I.M Diclofenac 75mg 12 hourly as rescue analgesia on request or when VAS ≥ 4. A standard postoperative analgesic regimen consisting of I.V Paracetamol 15mg/kg every 6 hours was commenced from PACU immediately on arrival of patients in both groups. The presence and severity of pain, nausea, and vomiting were assessed immediately on arrival in PACU and 2 hourly postoperatively according to proforma.
All patients were asked to score their pain at rest (VAS used) and on movement (Knee flexion where the pain was assessed using no pain, mild pain, moderate pain, and severe pain). Pain severity at rest was assessed using a visual analog scale (VAS, 10cm unmarked line in which 0cm = no pain and 10cm = worst pain imaginable) as shown in Appendix I. Nausea and vomiting were assessed using the following (minimal = 0, moderate =1, profuse =2) as shown in appendix II. The sedation score was measured using the Ramsay sedation scale (awake, anxious, and agitated =1, awake, cooperative, and tranquil = 2, asleep but respond to verbal commands only=3, asleep but brisk response to a loud auditory stimulus or light glabellar tap=4, asleep but sluggish response to loud auditory stimulus or light glabellar tap=5, asleep and no response =6) as shown on appendix III. Antiemetics (IV ondansetron 4mg) was administered for nausea or vomiting.
Postoperatively, vital signs (Heart rate, respiratory rate, blood pressure, and oxygen saturation) were measured 4 hourly for 12 hours as shown in the proforma. The study ended 12 hours after TAP blockade.
The primary outcome was the effect of morphine and TAP block on VAS Scores. The secondary outcome measured was the effect of morphine and TAP block on the time to first request for analgesia, patient satisfaction, and side effects associated with morphine and the local anesthetic agent used for TAP block.
2.3 Sample Size Calculation
The sample size formula was based on the Carney Method used to calculate the sample size. n = (u + v) 2 (P1 (1-P1) + P2 (1 –P2) (P1 -P2)2
n = Minimum sample size
P1 = Expected prevalence = 20%
P2 = Prevalence from a previous study = 5%
v = Percentage point of the normal distribution corresponding to the two sided significant level of 5% (v = 1.96)
u = One-sided percentage point of normal distribution where power equals
probability of finding a significant result using the power of 80% (u = 0.84)
n = (1.96 + 0.84)2 (0.20(1-0.20) +0.50 (1-0.50) (0.15)2
n = (7.84) (0.16 + 0.0475) = 1.6268
0.0225 0.0225 n = 72.3;
which was approximately 72 respondents. Then 10% attrition was added to the calculated sample size. This made my sample size to be 80, hence 40 respondents were used per group.
2.4 Statistical analysis:
The data collected were analyzed using the Statistical Product and Service Solution (SPSS) version 22.0. The data was summarized and presented as tables and charts. Chi-square test and level of significance were used to determine the association between categorical variables. Student t-test was used to test continuous variables, level of significance was set at 0.05.
The heart rate, Oxygen saturation, systolic blood pressure, diastolic blood pressure, and respiratory rate in both TAP block and morphine groups were recorded as mean ± standard deviation. A p-value less than 0.05 was considered statistically significant.
2.5 Ethical Consideration
Ethical approval was obtained from the Ethical and Research Committee of LAUTECH Teaching Hospital with approval number: LTH/EC/2016/06/23/275. The aim of the study was explained to the participants. Each participant was informed about the right to withdraw their consent and stop participating at any time without any form of prejudice. Privacy and confidentiality were maintained and written informed consent was also obtained from the participants.
3. RESULTS
A total of 80 participants were enrolled in the study, with 40 participants randomized to the TAP group and 40 participants to the morphine group. Following randomization, all the participants completed the study as allocated.
Enrollment Assessed for eligibility (n=80) Excluded (n=Nil) Declined to participate (n=Nil) Randomized (n=80)
Allocation
Allocated to TAP group intervention (n=40) Allocated to Morphine intervention group (n=40) The TAP group Received 20mls of 0.25% block on each side while morphine group received 20mls Normal saline on each side +IV morphine 4mg 4hourly Discontinued intervention (n-Nil) Follow Up for 12 hours discontinued intervention (n-Nil) Analysed (n=80) Excluded from analysis (n-Nil)
The patients’ age range in the TAP group was 18-38years with a mean of 26.05±5.67 years which was similar to a range of 17-37years with a mean of 25.85±6.06 years in group B (Morphine group). Mean gestational age was 38.39±2.62weeks in group A with a range of 34-41 weeks while in Morphine Group it was 38.66±8.26 weeks with arange of 37-40 weeks. The mean weight was 58.75±4.92kg in group A with a range of 51-89kg and 55.83±3.13 kg in group B with a range of 50-88kg. Table 1 shows the baseline socio- demographic characteristics of the study population. There was no significant difference between the randomized groups for any socio- demographic characteristics (age, education level, religion, BMI, gestational age, and parity).
The mean time to first analgesic request was longer in the TAP group 6.9±1.7hours compared to the Morphine group 5.7±1.4hours. This difference was statistically significant between the groups studied (p=0.000).
In Table 4, using the Likert Scale, 70% of the TAP group had a high level of satisfaction with their pain control while only 57.5% of the morphine group had a high level of satisfaction. This however was not statistically significant.
4. DISCUSSION
Pain management following cesarean section remains a challenge as the acceptable method of analgesia must be efficacious, safe, and with minimal side effects. Recently the quest to develop a regional method for pain management that is devoid of side effects associated with opioids has been the focus of pain managers.
This study compared the effects of TAP block with morphine on postoperative pain relief following elective Caesarean sections. The results showed that patients who received TAP block had better pain relief at rest and on movement, had better patient satisfaction, and had fewer side effects than patients in the morphine group. This efficacy of TAP block in this study tallies with the findings of Desale et al [13] and Srivastava et al
[14] where one group had a TAP block and the other group had no TAP block after Caesarean section, they discovered that pain scores were significantly lower in the TAP group (VAS of 3 and below) both at rest and on movement. This showed that TAP block is efficacious in post- caesarian section pain management. The findings of this study are also comparable to the findings of Maitreyi et al [15] in which ultrasound-guided TAP block with ropivacaine and saline were administered in addition to other routines (Paracetamol and Tramadol). The VAS score with the ropivacaine TAP group and the time of request for first analgesia was also prolonged, demonstrating the efficacy of TAP block using a local anesthetic agent.
The superiority of TAP showed in this study is not in tandem with the findings of Emre et al [16] where ultrasound-guided TAP block was compared to Intravenous morphine using a PCA machine. In the Emre et al study, there was no difference in the VAS score of the two methods used. This result is likely due to higher volume (30mls) used in their TAP block and PCA administration of morphine leading to similar efficacy in the two groups. The VAS score in this study is also different from the findings of McMorrow et al [17] in which TAP block was compared with spinal morphine. In that study, the authors discovered lower VAS scores in the morphine group, this is probably because of the potentiating effect of the 100 ug morphine added to the bupivacaine for spinal anesthesia coupled with the fact that morphine is effective in the management of both somatic and visceral pain while TAP block may be managing only the somatic pain.
In this study, VAS scores both at rest and on movement were similar on arrival at PACU in both groups. This is probably because spinal anesthesia was still effective. However, VAS scores were significantly lowered in the TAP group compared to the morphine group between 2 hours and 8 hours postoperatively. This is probably because the TAP block appears to still be effective within this period while the analgesic effect of spinal anesthesia would have worn off. However, VAS scores were also similar at the 12- hour post-operative time interval, this is likely because the TAP block effect has reduced, both groups were also given rescue analgesia on account of moderate pain, and these may be responsible for the similar VAS scores seen at 12 hours. This is similar to findings in Srivastava [14] in which one group received a TAP block while the other received no block. NRS scores for pain at rest and on movement were similar on arrival at PACU in both groups and NRS scores were lower at all times from 0 hours to 24 hours in the TAP group. This is probably because of the analgesic effect of IV diclofenac 75mg 8 hourly with IV Tramadol through PCA administered was still effective in both groups on arrival at PACU while TAP block played a potentiating role on other analgesics to make it effective till 24 hours post- operative period. The result of the VAS score in this study is similar to Salugna et al [18] in which patients who had total abdominal hysterectomy under general anesthesia were randomized into two groups. One group was given a TAP block with bupivacaine while the other group was given normal saline. They discovered that VAS scores in the immediate postoperative period both at rest (median VAS in TAP group vs. Placebo; 3mm Vs.27mm respectively) and with movement (median VAS score in TAP group vs. placebo; 8mm Vs.35mm respectively) were significantly lower in TAP block group with bupivacaine.
The time to first analgesic request in this study (6.9 hours) in the TAP group was slightly more prolonged than the morphine group(5.7hours) which also connotes better efficacy when the two are compared. The time to first rescue analgesia of the TAP group of this study though longer than the morphine group is still shorter than what was obtained in the Martreyi et al [15] (9.5 hours) study, despite a similar methodology. The difference seen may be due to the use of ultrasound for identification instead of landmark technique used in this study. Also, Srivastava et al [14]in a similar study reported a different result compared to this study. In the Srivastava et al [14] studies, the time to first analgesic request was 12 hours which is almost double the hour obtained in this study. The difference in these findings may be because they administered IV diclofenac 75mg 8 hourly coupled with IV tramadol 1mg per hour through PCA were most likely responsible for the prolonged time to first analgesic request when compared to this study where IM diclofenac was administered 12 hourly. This study is comparable to Jadon et al [19] in which a group received a TAP block with bupivacaine while the other group received a TAP block with normal saline. They discovered that the time to the first analgesic request was longer (11 hours) than the result in this study (6.9 hours). This could be because Jadon et al [19] also used an ultrasound-guided TAP block which allowed them to have a dense and prolonged block than this study. This is different from McMorrow et al [17] in which the time to first analgesic request was longer in the spinal morphine group than the TAP block group. This may be because spinal morphine will block at nerve routes effectively blocking both somatic and visceral pain while TAP block using bupivacaine alone may only be effective on somatic pain.
The two groups in this study experienced PONV at various degrees at different times. The morphine group had a higher incidence of PONV compared to the TAP group. At 6 hours postoperative, a greater percentage of patients in the TAP group had minimal PONV while all patients in the morphine group had PONV at various degrees. This is comparable to the study of Srivastava [14] who reported an incidence of PONV in the two study groups (TAP group and non-TAP group) although at a lesser incidence in the TAP group. The incidence of PONV in the Srivastava [14] study cannot be completely linked to the TAB block as all the patients had tramadol infusion (opioid) which has been documented as a major risk factor for PONV. The incidence of PONV in this study is also similar to the findings of Emre et al [16] in which the incidence of PONV was higher in the morphine group at the 30th minute but no difference in the first hour likely due to the emetic effect of tramadol given to the morphine group before extubation.
Pruritus and local anesthetic toxicity were also assessed but there was no record of any throughout the study period. This is similar to Sulagna et al [18] and Desale et al [13]. In Desale et al [13], no patient had pruritus in the TAP group but only one patient had pruritus in the control group with a score of 1. This is different from McMorrow et al [17] in which pruritus was more in the spinal morphine group due to the side effects of morphine.
In this study, the majority of the patients who had TAP block had a high level of satisfaction with pain relief while about half of the morphine group had the same level of satisfaction. This showed that the two methods are efficacious with better satisfaction with the TAP block group. This is similar to Woldehaimanot et al [20] in which 50% of the patients were adequately satisfied with their pain management. This is similar to the study by Jadon et al [19] and Srivastava [14] in which maternal satisfaction score was significantly higher in the TAP group compared to the control group with a p-value of 0.0002. This is not in tandem with the findings of McMarrow et al [17] in which there was no difference in patient satisfaction due to the side effects of spinal morphine which negatively influenced the patient’s satisfaction despite effective pain relief.
4.1: Conclusion
This study showed that patients who received TAP block had better pain relief and were more satisfied than those who received morphine as their analgesic.
Patients who received TAP block were more satisfied with their pain relief than those who received parenteral morphine.
4.2: Recommendations
Multimodal analgesia technique involving a combination of systemic analgesics with nerve
block like TAP block for postoperative pain control in Caesarean section as used in this study is recommended to ensure adequate pain relief, preservation of respiratory function, and patient satisfaction.
TAP block is an easy technique to learn and its practice should be encouraged in the analgesic armamentarium of multimodal technique.
4.3: LIMITATION
The ultrasound-guided TAP block is a better technique to obtain a higher success rate and would have been preferred but the equipment was not available. The use of PCA could have made morphine administration more accurate in the postoperative period.
Acknowledgment
We want to thank the Department of Anaesthesia and the Department of Obstetrics and Gynecology at Uniosun Teaching Hospital Osogbo for supporting this study. Further appreciation goes to the participants and the research assistants. Funding No funding was received for the study.
Author’s contributions
Folami Emmanuel Oladayo: Conceptualization, Validation, Resources, Formal analysis, Investigation, Methodology, Data curation, Visualization, Writing original drafts and Supervision.
Adelekan Adesoji Adebayo: Data curation, Formal analysis, Methodology, Writing-Review and Editing.
Afolabi Adegboyega Segun: Data curation, Formal analysis, Methodology, Writing-Review and Editing.
Folami Roseline Olufunmilola: Data curation, Formal Analysis, Methodology, Writing-Review and Editing.
Awodele Kehinde: Data curation, Formal Analysis, Methodology, Writing-Review, Editing, and Supervision.
Omopariola Samuel Olubunmi: Data curation, Formal Analysis, Methodology, Writing-Review Editing and Supervision.
Asafa Qozeem Opeyemi: Data curation, Formal Analysis, Writing-Review Editing and Supervision.
Akinwale Oladayo Damilola: Data curation, Methodology, Writing-Review Data Analysis, Editing and Supervision.
Farinloye Emmanuel Oludele: Data curation, Formal Analysis, Methodology, Writing- ReviewEditing and Supervision.
Conflict of Interest
The authors declare no conflict of interest
TABLE 1: COMPARING THE DEMOGRAPHIC AND CLINICAL DATA AND THE TYPE OF ANALGESIC TECHNIQUE
| TAP (%) | MORPHINE (%) | X2 VALUE | p-VALUE | |
|---|---|---|---|---|
| Age group (years) | ||||
| ≤20 | 12(15.0) | 10(12.5) | 2.848 | 0.583 |
| 21-25 | 8(10.0) | 8(10.0) | ||
| 26-30 | 10(12.5) | 14(17.5) | ||
| 31-35 | 8(10.0) | 4(5.0) | ||
| 36-40 | 2(2.5) | 4(5.0) | ||
| Education Level | ||||
| No Formal Education | 2(2.5) | 4(5.0) | 3.098 | 0.377 |
| Primary | 6(7.5) | 11(13.8) | ||
| Secondary | 14(17.5) | 12(15.0) | ||
| Tertiary | 18(22.5) | 13(16.2) | ||
| Religion | ||||
| Christianity | 12(15.0) | 17(21.2) | 1.352 | 0.245 |
| Islam | 28(35.0) | 23(28.8) | ||
| BMI | ||||
| Normal | 32(40.0) | 36(45.0) | 1.569 | 0.21 |
| Overweight | 8(10.0) | 4(5.0) | ||
| Residency | ||||
| Rural | 14(17.5) | 19(23.8) | 1.289 | 0.256 |
| Urban | 26(32.5) | 21(26.2) | ||
| Age (Years) | 26±5.67 | 25.85±6.06 | 0.879 | |
| Weight (kg) | 58.75±4.92 | 55.83±3.13 | 0.2 | |
| Height (m) | 1.57±0.11 | 1.56±0.09 | 0.571 | |
| BMI (kg/m2) | 24.05±2.80 | 23.19±2.22 | 0.129 | |
| Gestational age | ||||
| 38.39±2.62 | 38.66±8.26 | 0.063 | ||
| (weeks) | ||||
| ASA I:II ratio | 15.25 | 19.21 | 0.086 | |
| Parity | ||||
| Nullparity | 4(10.0) | 6(15.0) | ||
| Multiparity | 30(75.0) | 28(70.0) | 1 | |
| Grand multipara | 6(15.0) | 6(15.0) |
Figure 1: Trend of Post-Operative VAS between the study groups
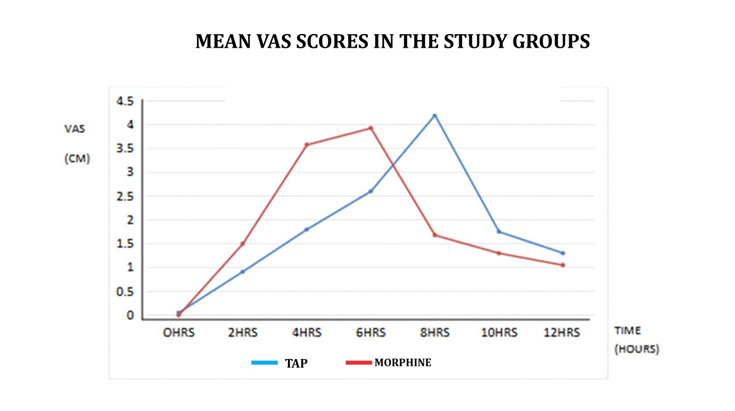 The VAS scores in the two groups were almost the same at PACU, at 2hrs, 4hrs, and 6hrs assessment, the TAP group had reduced VAS scores compared to the Morphine group up until the 7hrs assessment, although the Morphine group appeared better from the 7th hour and thereafter VAS score declined till the 12th hour in both groups.
The VAS scores in the two groups were almost the same at PACU, at 2hrs, 4hrs, and 6hrs assessment, the TAP group had reduced VAS scores compared to the Morphine group up until the 7hrs assessment, although the Morphine group appeared better from the 7th hour and thereafter VAS score declined till the 12th hour in both groups.
Table 2: Pain Severity Distribution on Movement (knee flexion) between the Study Groups
| VARIABLE | TAP (%) | MORPHINE (%) | X2 VALUE | P VALUE | |
|---|---|---|---|---|---|
| PACU PAIN | No Pain | 38(95.0) | 40(100.0) | 2.051 | 0.152 |
| Mild Pain | 2(5.0) | 0 | |||
| 2 HRS | No Pain | 16(40.0) | 2.(5.0) | ||
| Mild Pain | 22(55.0) | 38(95.0) | 17.156 | 0 | |
| Moderate Pain | 2(5.0) | 0 | |||
| 4 HRS | No Pain | 4(10.0) | 2(5.0) | ||
| Mild Pain | 36(90.0) | 5(12.5) | 57.106 | 0 | |
| Moderate Pain | 0 | 33(82.5) | |||
| 6 HRS | No Pain | 0 | 5(12.5) | ||
| Mild Pain | 40(100.0) | 2(5.0) | 72.381 | 0 | |
| Moderate Pain | 0 | 33(82.5) | |||
| 8 HRS | Mild Pain | 2(5.0) | 37(92.5) | 61.288 | 0 |
| Moderate Pain | 38(95.0) | 3(7.5) | |||
| 10 HRS | Mild Pain | 40(100.0) | 37(92.5) | 3.117 | 0.077 |
| Moderate Pain | 0 | 3(7.5) | |||
| 12 HRS | No Pain | 40(100.0) | 40(100.0) | - | - |
The TAP group had better pain control up until the 10th hour’s assessment when all the TAP group had mild pain and 7.5% in the morphine group had moderate pain.
3.2: Assessment of Side Effects
Table 3: Comparison of Incidence of Nausea and Vomiting between the Study Groups
| VARIABLE | TAP (%) | MORPHINE (%) | X2 VALUE | P VALUE | |
|---|---|---|---|---|---|
| PACU PONV | Minimal | 38(95.0) | 38(95.0) | 0 | 1 |
| Profusely | 2(5.0) | 2(5.0) | |||
| 2 HRS | Minimal | 38(95.0) | 40(100.0) | 2.051 | 0.152 |
| Profusely | 2(5.0) | 0 | |||
| 4 HRS | Minimal | 38(95.0) | 28(70.0) | 15.515 | 0 |
| Moderate | 0 | 12(30.0) | |||
| Profusely | 2(5.0) | 0 | |||
| 6 HRS | Minimal | 38(95.0) | 11(27.5) | 39.211 | 0 |
| Moderate | 0 | 19(47.5) | |||
| Profusely | 2(5.0) | 10(25.0) | |||
| 8 HRS | Minimal | 8(30.0) | 13(32.5) | 2.782 | 0.245 |
| Moderate | 30(75.0) | 23(57.5) | |||
| Profusely | 2(5.0) | 4(10.0) | |||
| 10 HRS | Minimal | 10(25.0) | 21(52.5) | 0.592 | 0.037 |
| Moderate | 28(70.0) | 17(42.5) | |||
| Profusely | 2(5.0) | 2(5.0) | |||
| 12 HRS | Minimal | 22(55.0) | 34(85.0) | 9.117 | 0.01 |
| Moderate | 16(40.0) | 6(15.0) | |||
| Profusely | 2(5.0) | 0 |
In Table 4, at 4 hours, 95% of TAP group had minimal PONV with 5% being profuse. Morphine group had 70% minimal PONV and 30% moderate. At 6 hours, 10 (25%) in the Morphine group versus 2 (5%) in the TAP group had profuse vomiting and were given IV ondansetron 4mg. This was statistically significant with a p-value < 0.000. At 12 hours larger percentage of the Morphine group had minimal PONV with half of the patients in the TAP group having the same experience.
Table 4: Level of Satisfaction of Patients with Analgesic Technique between the Study Groups using the Likert Scale
| Variable | TAP | MORPHINE | Chi- | Df | p- | |
|---|---|---|---|---|---|---|
| square | value | |||||
| Number of Patients (%) | Number of Patients (%) | Total | 1.352 | 1 | 0.244 | |
| Low level of | 12 (30.0) | 17 (42.5) | 29 (36.2) | |||
| satisfaction | ||||||
| High level of | 28 (70.0) | 23 (57.5) | 51 (63.8) | |||
| satisfaction | ||||||
| Total | 40 (50.0) | 40 (50.0) | 80 -100 |
REFERENCES
Srinivasa N. Raja, Daniel B. Carr, Milton Cohen, Nanna B. Finnerup et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges and Compromises 2020;7:1-7
Apfelbaum J.L, Chen C, Mehta S.S, Gran T.J. Postoperative pain experience: Results from a National Survey Suggest Postoperative pain continues to be undermanaged. Anesth 2003:97:534-540.
Ma N, Duncan JK, Scarfe AJ, Schuhmann S, Cameron AL. Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: A systematic review and meta-analysis. J Anesth 2017; 31(3): 432-52.
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. Journal of pain research. 2017 Sep 25:2287-98.
Katzman JG, Rollin Mac Gallagher. Pain: The Silent Public Health Epidemic. Journal of Primary Care & Community Health [Internet]. 2024 Jan 1;15. Available from: https://pubmed.ncbi.nlm.nih.gov/38742616/
Horn R, Kramer J. Postoperative Pain Control [Internet]. PubMed. Treasure Island (FL); 2022.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK544298/
Lorentzen V, Hermansen IL, Botti M. A prospective analysis of pain experience, beliefs and attitudes, and pain management of a cohort of Danish surgical patients. European Journal of Pain. 2012 (2):278-88.
Stephens J, Laskin B, Pashos C, Pena B, Wong J. The burden of acute postoperative pain and the potential role of the COX-2-specific inhibitors. Rheumatology. 2003; 42(suppl_3):40-52.
Klopper H, Andersson H, Minkkinen M, Ohlsson C, Sjöström B. Strategies in assessing post- operative pain—A South African study. Intensive and Critical Care Nursing. 2006 Feb 1;22 (1):12-21.
White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. AnaesthAnalg. 2005; 101: S5-S22.
Sharma S, Hashmi MF, Bhattacharya PT. Hypotension [Internet]. Nih.gov. StatPearls Publishing 2023.Available from: https://www.ncbi.nlm.nih.gov/books/NBK499961/
Good ED, Jongnarangsin K. Bradycardia. Practical Cardiology: Evaluation and Treatment of Common Cardiovascular Disorders. 2020:213-23.
Desale T.K, Waltraud E and Habteselassie Z.B Transversusabdominis plane block after Cesarean section in an area with limited resources. South African Journal of Anaesthesia a nd Analgesia. 2017:23:90-95.
Srivastava U, Verma S, Singh TK, Gupta A, Saxena A, Jagar KD, Gupta M. Efficacy of trans abdominis plane block for post-cesarean delivery analgesia: A double-blind, randomized trial. Saudi journal of anesthesia. 2015 ;9(3):298-302.
Mankikar MG, Sardesai SP, Ghodki PS. Ultrasound-guided transversus abdominis plane block for post-operative analgesia in patients undergoing caesarean section. Indian journal of
anaesthesia. 2016 ;60(4):253-7.
Emre E, Pinar K, Guniz M.K, Cigdem T et al. Comparison of transversus abdominis plane block and IV patient-controlled Analgesia after lower abdominal surgery. Turk J AnaesthReanim 2015 (43):24-28
McMorrow RC, Ni Mhuircheartaigh RJ, Ahmed KA, Aslani A, Ng SC, Conrick-Martin I, Dowling JJ, Gaffney A, Loughrey JP, McCaul CL. Comparison of transversus abdominis plane block vs spinal morphine for pain relief after Caesarean section. British journal of anesthesia. 2011; 106(5):706-12.
Sulagna B, Manjushree R, Tapes G, Souvik M, et al. Analgesic efficacy of transverses abdominis plane block in providing effective perioperative analgesia in patients undergoing total abdominal hysterectomy: A randomized controlled trial. J Anaesthesiol Clin Pharmacol 2014: 30 (3): 391-396.
Jadon A, Jain P, Chakraborty S, Motaka M, Parida SS, Sinha N, Agrawal A, Pati AK. Role of ultrasound-guided transversus abdominis plane block as a component of multimodal analgesic regimen for lower segment cesarean section: a randomized double-blind clinical study. BMC anesthesiology. 2018:1-7.
Woldehaimanot TE, Eshetie TC, Kerie MW. Postoperative pain management among surgically treated patients in an Ethiopian hospital. PloS one. 2014 9(7): e102835.
© 2025 Integrated Journal of Medicine and Medical Sciences. All rights reserved.
